Effective Periodontal Disease Treatment: What to Expect and How It Works
Periodontal disease, also known as gum disease, affects the tissues that surround and support the teeth. It’s a common yet serious condition, often caused by poor oral hygiene leading to bacterial infections. If left untreated, it can result in severe damage to the gums, bones, and teeth. Fortunately, modern periodontal disease treatments can effectively manage and reverse the progression of the condition. This article will explore the treatment process, what you can expect, and how these methods work to restore gum health.
Understanding Periodontal Disease
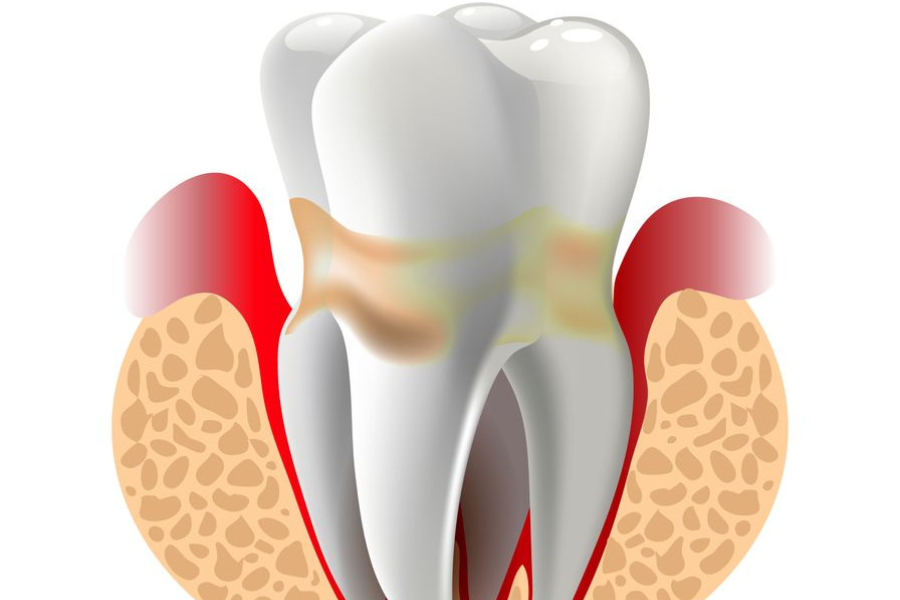
Before diving into treatment, it’s crucial to understand what periodontal disease is and how it progresses. Periodontal disease typically occurs in two stages:
- Gingivitis: The initial stage of gum disease, where gums become inflamed and may bleed easily. At this stage, no bone or tissue damage has occurred, and the condition is reversible.
- Periodontitis: If gingivitis is left untreated, it can advance to periodontitis, where the inner layer of the gum and bone pull away from the teeth, forming pockets that can become infected. Over time, this can lead to bone loss and tooth mobility, and eventually, tooth loss.
Key symptoms include swollen or bleeding gums, persistent bad breath, receding gums, and loose teeth. If any of these symptoms are present, it’s important to seek professional help as soon as possible.
Diagnosis of Periodontal Disease
Diagnosis is a vital first step in creating an effective treatment plan. A dentist or periodontist will begin by reviewing your medical history, assessing risk factors such as smoking or certain medications that could contribute to gum disease. A thorough examination of your mouth is next, which involves:
- Measuring gum pocket depth: Healthy pockets are usually between 1 and 3 millimeters deep. Pockets deeper than this may indicate periodontitis.
- Dental X-rays: These may be used to check for bone loss in areas where deeper gum pockets are found.
Once diagnosed, your dentist will categorize your condition as mild, moderate, or advanced, and recommend appropriate treatment.
Non-Surgical Periodontal Treatments
For mild to moderate periodontal disease, non-surgical treatments can often effectively manage and reverse the condition. Here are the most common non-surgical treatments:
- Scaling and Root Planing (Deep Cleaning)
Scaling and root planing is one of the most common and effective treatments for periodontal disease. This deep-cleaning procedure involves two steps:
- Scaling: Plaque and tartar are removed from above and below the gum line, especially in areas where pockets have formed.
- Root Planing: The tooth roots are smoothed out, which helps the gums reattach to the teeth and makes it harder for bacteria to accumulate.
This treatment may require local anesthesia and multiple visits depending on the severity of the disease. After the procedure, patients can expect some mild discomfort, swelling, or sensitivity, but these side effects are temporary.
- Antibiotic Therapy
Antibiotics may be used in conjunction with scaling and root planing to eliminate bacteria that cannot be removed mechanically. These can be administered in several ways:
- Topical antibiotics: Applied directly to the infected area in the form of gels, mouth rinses, or antibiotic fibers placed in the gum pockets.
- Oral antibiotics: In more severe cases, oral antibiotics may be prescribed to combat the infection systemically.
Antibiotics alone are not a cure for periodontal disease but can significantly aid in reducing bacterial infection and inflammation when combined with mechanical cleaning.
- Laser Therapy
Laser therapy is a less invasive treatment option that involves using a focused beam of light to remove inflamed gum tissue and bacteria. It can target specific areas with precision, leading to faster healing times and reduced discomfort compared to traditional methods. Laser treatment is especially useful for patients who cannot tolerate more invasive procedures or prefer a quicker recovery time.
Surgical Periodontal Treatments
In cases of advanced periodontal disease, non-surgical treatments may not be enough. Surgical options aim to restore the health of the gums and bone around the teeth. Here are the most common types of periodontal surgery:
- Flap Surgery (Pocket Reduction Surgery)
Flap surgery is performed when deep pockets between the gums and teeth have not responded to non-surgical treatments. The procedure involves lifting back sections of the gum tissue to expose the tooth roots for more thorough scaling and root planing. Afterward, the gum tissue is sutured back into place to reduce the size of the pockets, which helps prevent bacteria from accumulating.
Patients can expect some swelling and discomfort following flap surgery, but recovery generally occurs within a couple of weeks.
- Bone and Tissue Grafts
Bone and tissue grafts are often necessary if the periodontal disease has resulted in significant bone or tissue loss. These procedures include:
- Bone grafts: Small pieces of bone or synthetic material are placed in areas where bone loss has occurred, encouraging new bone growth.
- Soft tissue grafts: This procedure involves using tissue from the roof of your mouth or another donor source to cover exposed roots or build up receding gum lines.
- Guided tissue regeneration: A specialized membrane is placed between the bone and gum tissue to promote new bone and tissue growth.
Grafts can significantly improve the structure and function of the teeth and gums, preventing further deterioration and enhancing aesthetics.
- Bone Surgery
Bone surgery is used to smooth out shallow craters in the bone caused by moderate to advanced bone loss. After flap surgery, the bone around the tooth is reshaped to reduce areas where bacteria can thrive. This treatment is often combined with other periodontal surgeries to create a more stable foundation for the teeth.
Post-Treatment Care and Maintenance
Periodontal disease is a chronic condition that requires ongoing care and maintenance to prevent recurrence. After treatment, you’ll need to follow a strict oral hygiene routine and attend regular dental check-ups. Key post-treatment steps include:
- Daily brushing and flossing: Brush twice a day with fluoride toothpaste and floss at least once a day to remove plaque and prevent new pockets from forming.
- Regular dental visits: Professional cleanings every 3 to 6 months will be essential in maintaining the health of your gums.
- Lifestyle changes: If you smoke, quitting will significantly improve your gum health and reduce the risk of future infections.
Additionally, your dentist may recommend antimicrobial mouthwashes or other products to help control bacteria and promote healing.
Effective periodontal disease treatment requires a combination of professional dental care, lifestyle changes, and diligent oral hygiene. Whether treated non-surgically or through surgery, the goal is to stop the progression of the disease, restore gum health, and preserve your natural teeth. If you suspect you have gum disease, don’t wait—early diagnosis and treatment can prevent serious complications and help you maintain a healthy smile for life.